Imagine a tiny muscle that controls the flow of digestive juices in your body – sounds like a minor player, right? Wrong. The Sphincter of Oddi is a critical gatekeeper in your digestive system, and when it malfunctions, life can become a nightmare of pain and digestive chaos.
What Exactly Is the Sphincter of Oddi?
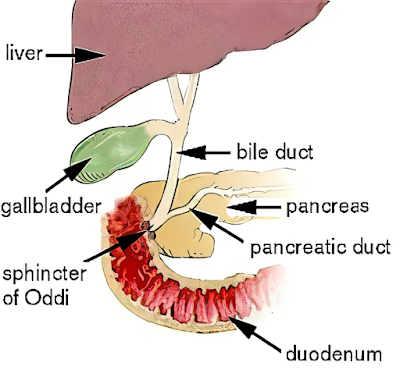
According to the Cleveland Clinic, this is a muscular valve that controls the flow of bile and pancreatic juices into the small intestine. Think of it like a traffic controller for digestive fluids – when it works correctly, everything flows smoothly. When it doesn't, traffic comes to a painful standstill.
The Mysterious World of Sphincter Dysfunction
Experts aren't entirely sure what causes Sphincter of Oddi Dysfunction (SOD), but several theories exist:
- Scarring from previous surgeries
- Trauma to the area
- Congenital issues with the sphincter
- Potential connections to microlithiasis (tiny gallstones)
Recognizing the Symptoms
The hallmark of SOD is unmistakable: severe, recurring abdominal pain. Specifically:
- Intense pain in the upper right side of the abdomen
- Pain that can last from minutes to hours
- Often triggered after eating, especially fatty foods
- Potential nausea and vomiting
Diagnosis: Not as Simple as It Sounds
Diagnosing SOD is complex. It typically involves:
- Detailed medical history
- Physical examination
- Blood tests
- Imaging studies (ultrasound, CT scan, MRI)
- Specialized testing like ERCP (Endoscopic Retrograde Cholangiopancreatography)
Treatment Approaches
Recent 2024 research has highlighted several treatment strategies:
Medication Management
- Calcium channel blockers
- Antispasmodic medications
- Nitrates to relax the sphincter
Surgical Interventions
- Sphincterotomy (cutting the sphincter to improve flow)
- Potential endoscopic procedures
Lifestyle Modifications
- Avoiding alcohol
- Quitting smoking
- Limiting high-fat foods
- Maintaining a healthy weight
- Managing cholesterol levels
Potential Complications
If left untreated, SOD can lead to:
- Chronic pain
- Recurrent pancreatitis
- Bile duct inflammation
- Potential long-term digestive issues
Living with SOD: A Patient's Perspective
This isn't just a medical condition – it's a life-altering experience. Patients often describe a journey of frustration, pain, and finally, understanding. The key is working closely with healthcare providers to develop a personalized management plan.
Emerging Research
A fascinating 2024 study continues to explore the intricate mechanisms of sphincter dysfunction, offering hope for more targeted treatments in the future.
When to Seek Help
Don't ignore persistent abdominal pain. If you experience:
- Recurring upper right abdominal pain
- Digestive issues after eating
- Unexplained nausea or vomiting
Consult a gastroenterologist who can provide a comprehensive evaluation.
The Road Ahead
SOD is a complex condition that requires patience, understanding, and a comprehensive approach. While it can be challenging, modern medicine offers more hope and better management strategies than ever before.
This article reflects current medical understanding as of April 2025. Always consult with a healthcare professional for personalized medical advice.